There are several terms commonly used “Accelerated Hypertension”, “Hypertensive Emergency”, “Malignant Hypertension”. They all have a very similar definition (ESC/ESH, NICE, ACEP)
Patient has both:
- Blood pressure: Systolic ≥180mmHg OR Diastolic ≥110mmHg (often >220/120mmHg)
- End-Organ Damage: Retinal Changes, Encephalopathy, Heart Failure, Acute Kidney Injury, etc.
Mortality has improved in recent years with 5yr survival of 80% if treated. However, untreated average life expectancy is 24 months.
Investigation (All suspected cases):
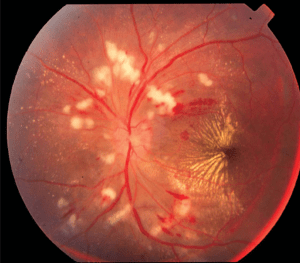
Blurring of the optic nerve , diffuse peripapillary cotton‐wool spots, flame‐shaped, hemorrhages, diffuse exudates, and. a macular star.
- ECG
- Bloods: FBC, U&E
- Urine: Dip (protein and blood), Microscopy, Pregnancy (if childbearing age)
- Fundoscopy: is a critical part of the diagnostic workup – Digital Retinal Imaging is the method of choice currently
Further Investigations (Specific Indications – not always in ED):
- Troponin (Suspected MI)
- BNP (Heart Failure)
- CXR (Pulmonary Oedema)
- CT Aorta (Suspected acute aortic disease e.g. aortic dissection)
- CT/MRI Brain (Nervous system involvement)
- Renal ultrasound (Renal impairment or suspected renal artery stenosis)
- Urine drug screen (Suspected methamphetamine or cocaine use)
Management

ACEP
Hypertensive Emergency Treatment
Disease Specific IV therapies recommended by (ESC/ESH) – but liaise with local speciality teams as these patients will need admission
| Clinical Indication | Target/Timing | First Line | Second Line |
|---|---|---|---|
| Malignant Hypertension | Several hours Reduce MAP by 20–25% | Labetalol/Nicardipine | Nitroprusside |
| Hypertensive Encephalopathy | Immediately Reduce MAP by 20–25% | Labetalol/Nicardipine | Nitroprusside |
| Acute Coronary Event | Immediately Reduce sBP <140mmHg | Nitroglycerine/Labetalol | Urapidil |
| Acute Cardiogenic Pulmonary Oedema | Immediately Reduce sBP <140mmHg | Nitroglycerine/Nitroprusside with Fruosemide | Urapidil with Furosemide |
| Aortic Dissection | Immediately Reduce sBP <120mmHg AND HR <60bpm | Nitroglycerine/Nitroprusside | Labetalol/Metopralol |
| Eclampsia, Severe Pre-Eclampsia/HELLP | Immediately Reduce sBP <160mmHg AND dBP <105mmHg | Labetalol/Nicardipine with Magnesium Sulphate | Consider Delivery |
Non-Emergent Hypertension Treatment – NICE
- Oral therapy is normally sufficient
- Calcium Channel Blockers are probably our 1st line in ED – as ACEi require renal monitoring
- If already on extensive Antihypertensive therapy – Medical review will be required
- If Adjusting/Starting oral antihypertensives there is no need for patient to wait in ED for BP to drop
- Life style advice is also useful
- Discharge for GP Follow-Up within 7 days
Phaeochromocytoma! (suspected cases require urgent medical review)
- Episodic symptoms (the 5 ‘Ps’):
- Paroxysmal hypertension,
- Pounding headache,
- Perspiration,
- Palpitations
- Pallor
- Blood Pressure may be: Labile OR Surges precipitated by drugs (e.g. β-blockers, metoclopramide, sympathomimetics, opioids, and tricyclic antidepressants)
- Skin inspection: cafe-au-lait patches of neurofibromatosis
Tests:
- CT/MRI
- Plasma or 24hr urinary fractionated metanephrines
Treatment:
- First Line Blood pressure managment α- adrenergic receptor blockers
- Don’t use β-Blockers Alone (risk of hypertension)
- Surgical management is the ultimate treatment
